Health
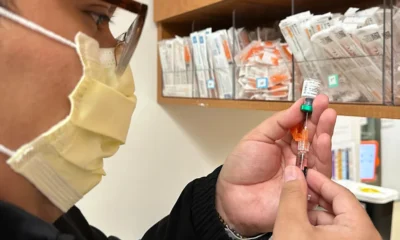
Confronting Mpox in East Africa’s Conflict Zones: Strategies for a Critical Response

As Mpox Threatens to Worsen the Crisis, Key Actions Needed to Address the Outbreak Amidst Regional Conflicts
As the mpox outbreak continues to surge through East Africa, including Kenya, Rwanda, Burundi, and Uganda, the situation has reached a fever pitch. The epidemic, which began in the Democratic Republic of Congo in January 2023, was declared a public health emergency by the Africa Centres for Disease Control and the World Health Organization in August 2024. The spread of this viral disease is particularly alarming in regions plagued by conflict.
The intersection of mpox and ongoing or recent conflicts presents a grim scenario. War-torn countries in East Africa and the Horn, such as Sudan and Somalia, face catastrophic healthcare challenges. In Sudan, over a year of relentless conflict has crippled 70% of health facilities, leaving the remaining ones besieged by attacks and shortages. Similarly, Somalia, grappling with decades of strife, has one of the world’s lowest childhood immunization rates. Ethiopia, with its recent Tigray conflict, saw its healthcare system in tatters, a crisis that our research underscores.
The Tigray conflict (2020-2022) offers a sobering lesson. The federal blockade led to a collapse of the healthcare system, massive displacement, and severe damage to health facilities. Our research from 2021 revealed that 39% of infants received no basic vaccinations due to the war. This was further corroborated by a recent WHO report, highlighting simultaneous outbreaks of several infectious diseases in Sudan’s states.
These past experiences underscore the dire need for a robust response to the mpox outbreak in conflict zones. Here’s how we can effectively manage the situation:
1. Integrate Vaccine Distribution with Humanitarian Aid: Efficient deployment of mpox vaccines requires blending with broader humanitarian efforts. Coordination ensures that vaccines are delivered alongside other essential supplies, leveraging existing logistical frameworks to reach those in need.
2. Engage Local Communities: Building trust with local communities is crucial. By involving local leaders and residents, we can protect frontline workers from conflict-related dangers and foster acceptance of the vaccine. Establishing permanent vaccination teams from within these communities will enhance the response.
3. Collaborate with Military and Security Forces: Securing the safe delivery of vaccines may necessitate military escorts, similar to practices in humanitarian aid. This collaboration is vital to navigate conflict zones and ensure uninterrupted vaccine delivery.
4. Negotiate Access with Conflict Actors: Understanding and negotiating with the various factions controlling conflict areas can reduce operational risks. Securing physical access through dialogue with these groups is essential for effective vaccine distribution.
5. Address Transit and Cross-Border Vaccinations: Given the frequent displacement of populations in conflict zones, vaccinating at transit points is crucial. This approach will ensure that those moving across borders or fleeing violence are protected.
6. Deliver Vaccines to Refugee and Internally Displaced Person Camps: Special attention must be given to camps housing refugees and internally displaced persons. These areas are particularly vulnerable and require targeted vaccination efforts to prevent the spread of mpox.
In conclusion, the mpox outbreak in East Africa’s conflict zones demands a multifaceted response. By integrating vaccination efforts with humanitarian aid, engaging local communities, and collaborating with military forces, we can mitigate the impact of this deadly virus. The lessons from past conflicts, combined with strategic planning, will be pivotal in controlling the spread of mpox and safeguarding public health in these turbulent regions.
Health
How Somaliland’s Business Elite is Profiting from Your Funeral

In the shiny boardrooms of Hargeisa and the bustling docks of Berbera, a group of men are getting very rich. They drive the latest SUVs, they build the tallest hotels, and they are hailed as the “backbone of our economy.” But look closer at what they are selling you. Look at the rice, the milk, and the medicine.
The truth is darker: Somaliland’s business elite is currently engaged in the most profitable mass-poisoning in our nation’s history. They aren’t just selling products; they are selling slow-acting death, and they are doing it with a smile.
The $300 Million Milk Scam
Somaliland is a nation of livestock. We are the world’s exporters of goats and camels. Yet, every year, we hand over $300 million to foreign companies and local middlemen for “milk” that never saw a cow.
The liquid in those cartons is not milk. It is a chemical cocktail—white-colored water stabilized with additives to survive years in a shipping container without refrigeration. Real milk dies in days; this “poison” lives for three years on a shelf.
The irony is sickening. Saudi Arabia—a desert—imports our live animals because they want real nutrition. In return, we take their money and buy back containers of synthetic powder and liquid “milk” made in countries that don’t even have livestock. We are trading our lifeblood for their lab-made waste. One liter of this imported “poison” costs less than a dollar after taxes and shipping—that price alone should tell you it isn’t food. It is a health risk in a carton, and our children are the first victims.
The Rice Crisis: Arsenic on Every Plate
For years, we have trusted rice as our national staple. But as our families drain their life savings to fly to India for cancer treatment, we have to ask: What are we eating?
Dr. Cabdirisaaq Cartan has bravely broken the silence. Rice is a sponge for arsenic, a Group 1 carcinogen. In Somaliland, we don’t just eat rice; we consume mountains of it three times a day. We are importing low-grade, expired, and poorly stored Basmati from South Asia that would be rejected by any nation with a functioning health department.
While the “Business Kings” count their profits from these shipments, our people are developing bladder, skin, and lung cancers at rates never seen before. The silence from the Ministry of Health is bought and paid for by the very merchants who fill our warehouses with this toxic grain.
Repackaged Death: The Medicine Racket
Somaliland’s Crackdown: Yemeni Nationals Arrested for Repackaging Expired Medicine
If the food doesn’t kill you, the “cure” might. A recent police bust in Hargeisa uncovered Yemeni nationals repackaging expired drugs with fake labels from China. This isn’t an isolated incident; it is a business model.
When a “businessman” imports $9,000 worth of fake cartons to make expired medicine look new, he isn’t just a fraud—he is a murderer. People like Sado Mohamud, who suffered a stroke after taking a “new” prescription from an unregulated clinic, are the collateral damage of a market that favors volume over life.
The Cost of “Cheap”
Somalilanders are poor and vulnerable, and the rich man knows it. They tell you it’s “cheap” so you can afford to feed your family. But is it cheap when you have to sell your land to pay for a biopsy in Addis Ababa? Is it cheap when your child develops a mysterious rash or a fever from fake powdered milk?
These businessmen are killing the very market they want to make money from. A dead customer cannot buy rice. A sick nation cannot build an economy.
The merchants of Hargeisa have a choice: become honest builders of this nation, or continue being its undertakers. For the rest of us, the message is simpler: Stop buying your own funeral.
Somaliland: How Fake and Expired Medicines Are Putting Lives at Risk
Health
Addressing the Quiet Crisis of Antimicrobial Resistance in Somaliland

No outbreak. No alarm. Just medicines that stop working—and lives that quietly slip away.
By Dr. Fadumo Abdi, PhD
Antimicrobial resistance does not arrive with sirens. It does not trigger emergency press conferences or overwhelm hospitals overnight. Instead, it creeps in quietly—through infections that no longer respond, wounds that refuse to heal, and doctors forced to hesitate before prescribing medicines that once worked with certainty.
Across the world, health leaders now rank antimicrobial resistance (AMR) among the most serious threats to modern medicine. Yet in Africa—and particularly in Somaliland and the wider Somali region—it remains a hidden crisis. Not because it is rare, but because it is poorly measured, weakly regulated, and often ignored until treatment fails.
This is the invisible breach in our health system.
A Crisis Without a Headline
At its core, antimicrobial resistance is biology responding to misuse. Bacteria adapt. Pathogens evolve. Medicines lose their power. What was once routine care becomes a gamble.
According to World Health Organization, hundreds of thousands of deaths in Africa each year are linked to drug-resistant infections. The burden falls hardest where laboratory surveillance is weakest. In Somaliland, this reality plays out daily—recurrent urinary tract infections that defy first-line treatment, post-partum infections that escalate dangerously, and rising cases of sepsis that reflect not poor doctors, but failing tools.
Resistance here is not low. It is simply undocumented.
Why AMR Is Accelerating in Somaliland
The drivers of resistance in Somaliland are structural, not accidental.
Antibiotics are widely available without prescription, turning life-saving drugs into consumer goods. Informal pharmacies often serve as the first—and only—point of care for communities far from clinics. Treatment courses are cut short once symptoms fade, allowing the strongest bacteria to survive and multiply.
Compounding this is a diagnostic vacuum. Many facilities lack even basic laboratory capacity to identify pathogens or test drug sensitivity. Clinicians are forced to prescribe broad-spectrum antibiotics blindly—a practice that unintentionally fuels resistance.
Livestock adds another layer of risk. In a country where animals far outnumber people, antibiotics are heavily used in veterinary care, often without oversight. Resistant organisms move easily between animals, humans, and the environment—a classic One Health failure. The circulation of substandard and falsified medicines, degraded by heat and poor storage, further weakens treatment and accelerates resistance.
A Regional Pattern of Fragility
In 2019 alone, antimicrobial resistance was associated with more than one million deaths across Africa. It is quietly eroding progress against tuberculosis, pneumonia, and bloodstream infections.
In Somaliland, official data understates the problem. The absence of laboratory surveillance creates an illusion of safety. But clinicians know better. Resistance is present in wards and clinics—it is simply uncounted.
This is not just a medical issue. It reflects governance, regulation, education, water access, and supply chains. AMR threatens every newborn delivery, every surgical procedure, and the long-term credibility of our health system.
A Narrow Window to Act
Somaliland still has an opportunity—precisely because its health system is still evolving. Reform does not require dismantling entrenched bureaucracies. It requires focus.
The response must be clear and disciplined:
Regulatory oversight: End the unchecked sale of antibiotics and treat them as clinical tools, not retail items.
Diagnostic investment: Expand basic laboratory capacity so clinicians can treat with evidence, not guesswork.
One Health integration: Link human, animal, and environmental surveillance to close the loop through which resistance spreads.
Antimicrobial resistance is a test of leadership in the absence of spectacle. It demands coordination, foresight, and attention to details the public rarely sees.
The bacteria are adapting—silently and relentlessly. Whether Somaliland adapts in time will determine not just the future of its health system, but the safety of generations yet to come.
Health
Kenya Signs $2.5 Billion US Health Deal Amid Growing Fears Over Data Privacy

Kenya’s Landmark US Health Deal Exposes a New Era of Aid Politics — and a High-Stakes Fight Over Data Sovereignty.
Kenya’s decision to sign a $2.5 billion health agreement with the United States marks a dramatic shift in Washington’s foreign aid strategy and places Nairobi at the center of a new geopolitical contest over health security, national sovereignty, and the control of digital data.
The agreement — the first of its kind since President Donald Trump dismantled USAID and froze large portions of US foreign assistance — is being hailed by both governments as a blueprint for future partnerships across Africa.
Yet beneath the public ceremony lies growing unease about the price of accepting Washington’s new model of aid.
The deal, unveiled in Nairobi with President William Ruto and US Secretary of State Marco Rubio, commits the US to invest $1.7 billion over five years, while Kenya will contribute $850 million and gradually assume increasing responsibility.
It targets critical sectors — HIV/AIDS, malaria, tuberculosis, maternal care, polio eradication, and infectious disease preparedness — at a moment when global supply chains have tightened and developing countries face shortages of essential medicines following Trump’s aid overhaul.
For Washington, however, this agreement is more than a health partnership. It is a political instrument. Trump’s “America First Global Health Strategy” ties aid to direct government-to-government deals, bypassing NGOs and traditional aid networks while empowering US agencies to streamline oversight.
The shift also reinforces the administration’s strategic goal: to deepen alliances with governments aligned with US priorities and reduce financial flows to organizations it sees as wasteful or unaccountable.
But this new model has sparked immediate controversy in Kenya. Critics fear the agreement could grant the US access to real-time health databases containing sensitive personal information — including HIV status, TB treatment history, genomic data, vaccination records, and biometric files.
Kenya’s Health Minister Aden Duale insists only aggregated, de-identified data will be shared, dismissing concerns as misinformation. Yet the absence of a publicly released agreement has amplified distrust.
Legal scholars and civil society activists are now demanding transparency, arguing that data-sharing provisions must be explicitly stated to prevent potential abuse.
As whistle-blower Nelson Amenya put it: “We can’t safeguard what we can’t see.” Their fears reflect a global dilemma: as foreign aid becomes increasingly tied to digital infrastructure and data-driven surveillance, traditional questions about sovereignty and privacy take on new urgency.
Meanwhile, the US is presenting the deal as a reward for Kenya’s strategic partnership — particularly its leadership in the UN-backed mission in Haiti.
Rubio’s praise of Nairobi’s willingness to “step forward” underscores the political dimension of the partnership, where security cooperation, foreign policy alignment, and health investment converge.
More African countries are expected to sign similar agreements by year’s end, signaling that Washington’s aid revamp is just beginning.
Whether these deals strengthen national health systems or compromise digital sovereignty will depend on how transparently they are negotiated — and whether governments like Kenya’s can defend both their strategic interests and their citizens’ data rights.
Health
Inside Somalia’s Failing Hospitals as Donor Support Dries Up

Somalia’s Collapsing Hospitals Expose the Human Cost of Aid Cuts and Endless War.
MOGADISHU — When Yusuf Bulle carried his severely malnourished 3-year-old son from a remote village in southern Somalia to Mogadishu, Banadir Hospital was his only hope. “Where I come from, there is no hospital,” he said, standing in a crowded pediatric ward. After fifteen days, his child survived — but in much of Somalia, thousands of others are not as fortunate.
A nationwide collapse of Somalia’s already fragile health system is accelerating after the Trump administration’s dismantling of the U.S. Agency for International Development earlier this year, a decision that wiped out critical funding for clinics and frontline medical staff.
The result is a health crisis layered atop an ongoing war against al-Shabab and deep donor fatigue that is eroding the last functioning institutions in one of the world’s poorest countries.
Somalia’s deputy health minister, Mohamed Hassan Bulaale, said the cuts eliminated more than 6,000 health workers and affected up to 2,000 facilities — a devastating blow in a nation where basic care is already scarce. “Wherever you go, it’s donors that keep the hospitals alive,” he said.
Security Gains, Social Collapse
While deadly al-Shabab bombings have decreased under President Hassan Sheikh Mohamud’s “total war” campaign, the government’s overwhelming focus on security has drained attention from collapsing public services.
Civic leaders warn that the cost of military gains is becoming painfully clear in Mogadishu’s hospitals, where wards depend almost entirely on UN agencies and humanitarian groups to function.
Somalia’s Ministry of Health received $91 million in this year’s national budget — nearly double last year’s allocation — but analysts say the apparent increase masks a grim reality: almost all of the funding came from external donors. As Mahad Wasuge of the Somali Public Agenda put it, “Security remains the first priority. Everything else is an afterthought.”
In rural areas, “everything else” often means nothing at all.
Hospitals Held Together by Foreign Funding
At Banadir Hospital, the main public referral hospital in Mogadishu, even the unit for severely malnourished children depends entirely on donor money funneled through Concern Worldwide. Dr. Mohamed Haashi says 37 employees lost their jobs when U.S. aid was cut; only 13 remain, all funded by Concern. The milk, food, and medicine keeping children alive come from the same pipeline.
Across the city at De Martino Hospital — a century-old facility established during Italian colonial rule — administrators worry their lifeline will soon snap. Contracts with two humanitarian groups expire in late 2025. “Now it looks like donors are fatigued,” said the hospital’s director, Dr. Abdirahim Omar Amin, gesturing toward laboratory equipment purchased almost entirely through aid.
De Martino’s pediatric wing was treating dozens of children with diphtheria, a disease easily prevented by routine vaccination. But rural parents, fearing militant attacks on clinics, have stopped bringing their children in.
“Even the limited public hospitals that function rely almost entirely on donors,” said Wasuge. “The government gives no direct budget to keep them alive.”
A State Adrift
The story of Somalia’s hospitals mirrors the story of the state itself: structures shattered by decades of civil war, partially rebuilt by foreign funds, and perpetually one crisis away from collapse. After the fall of Siad Barre in 1991, many public buildings became shelters for the displaced. Some never reopened.
Today, the federal government operates from a heavily fortified enclave near Mogadishu’s airport, reliant on African Union peacekeepers, U.S. airstrikes, and foreign advisers in a country where multiple powers — from Turkey to Gulf states — compete for influence on the Indian Ocean and the Gulf of Aden.
Despite that geopolitical attention, Somalia has “no national healthcare plan,” said Mohamed Adam Dini, a parliamentarian from Puntland. “A lot of diseases are spreading unchecked. There is no political plan — so how can there be a health plan?”
For Somalis like Amina Abdulkadir Mohamed, who recently gave birth at De Martino because she knew she wouldn’t be asked to pay, the crisis is already personal. “I was told there is free medication,” she said. How long that remains true depends entirely on donors who are, increasingly, leaving.
Health
Is Our Rice Addiction Fueling Somaliland’s Cancer Crisis?

EXPOSÉ: Somaliland’s Daily Poison — Is a Contaminated Rice Supply Driving Our Cancer Surge?
WARYATV INVESTIGATION | HARGEISA — For years, rice has been the quiet ruler of the Somali kitchen: cheap, filling, familiar. But as cancer cases rise at an alarming pace and Somaliland families drain their savings traveling to India for treatment, a devastating question now hangs over the dinner table: Is our national staple slowly poisoning us?
A respected medical expert, Dr. Cabdirisaaq Cartan, has broken ranks with the silence in the health sector, urging the public to stop eating rice immediately—a warning he links directly to the country’s cancer spike and to widespread consumption of expired, poorly stored imports.
His message is blunt, and the science backing it is even harsher.
The Hidden Carcinogen Sitting in Every Somaliland Kitchen
Rice is uniquely efficient at absorbing arsenic, a toxic heavy metal classified globally as a Group 1 carcinogen. Because rice is grown in flooded conditions, it pulls arsenic out of the soil far more aggressively than other grains.
Across the world, more than 3.5 billion people depend on rice. But the danger becomes acute when it is eaten three times a day, every day — exactly the pattern in Somali households.
Long-term arsenic exposure is linked to higher rates of lung, bladder, and skin cancers, and a growing body of research shows impacts on heart disease, pregnancy outcomes, and child development.
Somaliland’s situation is even more alarming. We are not consuming small, occasional bowls of rice — we are consuming mountains of it, often from unknown suppliers, from warehouses with questionable storage conditions, and sometimes past the expiration date.
The Basmati Myth
Most rice imported into Somaliland markets — Basmati from South Asia — carries lower arsenic levels, but not safe levels. The largest long-term studies, including the California Teachers Study, found:
-
A measurable increase in breast and bladder cancer risk linked to regular rice consumption.
-
Scientists warned that populations like Somalis, who eat rice as a staple rather than a side dish, face significantly higher lifetime risk.
Even “low arsenic” rice becomes dangerous when eaten in the volumes common across Somaliland.
A National Silence — and a Public Paying the Price
Despite the warnings from Dr. Cartan, the Ministry of Health has issued no investigation, no data, no response. Berbera port continues to receive rice shipments with no mandatory arsenic testing, no transparent quality controls, and no public reporting.
Meanwhile, hundreds of Somaliland families go bankrupt each year seeking cancer care in India — the human cost of a crisis no one in government has bothered to confront.
Dr. Cartan also raised a painful truth: Somaliland’s media rarely investigates this kind of public health threat. Photo-ops with politicians dominate airtime, while potentially contaminated food continues entering the national market.
What Families Must Do — Starting Today
This is not fearmongering. It is a public safety alert.
Until the government enforces stricter controls, Somalilanders must protect themselves:
1. Reduce daily rice intake.
Replace it with millet (misago), corn, oats, barley, sorghum, or quinoa.
2. Wash and cook properly.
Rinse thoroughly, then cook rice in 6:1 water and drain the excess — a method proven to remove much of the arsenic.
3. Protect children and pregnant women.
They are most vulnerable to arsenic exposure. Their rice consumption should be strictly limited.
A National Health Emergency We Can No Longer Ignore
Cancer is destroying Somaliland households. The financial burden is crushing families. The silence from leadership is indefensible.
Dr. Cartan’s warning is not an attack on culture — it is a call for survival.
Somaliland must demand transparency, enforce food safety standards, and confront the deadly possibility that the very meal we trust most may be the one hurting us.
Health
Over Half a Million Blood Pressure Pills Recalled for Cancer-Linked Impurities

FDA Warns of Cancer-Linked Impurities in Popular Blood Pressure Medicine.
Health The U.S. Food and Drug Administration (FDA) has announced a major recall of more than 500,000 bottles of the blood pressure medication prazosin hydrochloride, citing the presence of N-nitrosamines, chemical compounds associated with an increased risk of cancer.
The recall, initiated by Teva Pharmaceuticals, applies to 1 mg, 2 mg, and 5 mg tablets of prazosin hydrochloride, an FDA-approved alpha-blocker commonly prescribed to treat high blood pressure and, in some cases, PTSD-related nightmares and prostate issues.
According to the FDA’s enforcement notice, the recall is categorized as a Class 2 event, meaning the medication “may cause temporary or medically reversible adverse health consequences,” though the likelihood of serious harm is considered remote.
The affected lots were found to contain elevated levels of N-nitrosamine impurities, specifically “N-nitroso Prazosin impurity C.” Nitrosamines are environmental contaminants found in water, certain foods, and cured meats, but at high levels in medications, they pose long-term carcinogenic risks.
The FDA emphasized that the danger arises primarily from sustained exposure over time, not short-term use.
While Teva and the FDA have not issued direct instructions for patients to discard the medication, pharmacists advise consumers to check the lot number on their prescription bottles and consult their doctor or pharmacist before making any changes.
“Stopping your blood pressure medication suddenly can be more dangerous than continuing it,” noted a Harvard Health report cited by the agency.
Teva has not confirmed how the impurities formed but said it is cooperating with regulators to remove affected products from circulation.
The FDA added that such impurities can develop during manufacturing or prolonged storage, particularly under certain temperature or chemical conditions.
Health experts recommend that patients continue their prescribed treatment until they speak with their healthcare provider. Pharmacists can help verify whether a specific batch number falls under the recall list available on the FDA website.
The recall underscores a growing concern in the U.S. pharmaceutical supply chain, where nitrosamine contamination has triggered multiple recalls over the past five years, including for blood pressure and diabetes medications.
For patients, vigilance remains key: check your lot number, contact your pharmacist, and seek medical guidance before stopping any medication.
Health
Unpacking the High Risk for Somali Mothers in Childbirth

A Common Procedure, A Dangerous Complication
A new study has brought to light a significant and alarming health risk for women in Somalia: low blood pressure during childbirth. Published in the journal BMC Pregnancy and Childbirth, the research focused on mothers undergoing cesarean sections at the Recep Tayyip Erdoğan Hospital in Mogadishu. The findings are stark. Of 320 women who received spinal anesthesia for the procedure, a staggering 79% experienced a severe drop in their blood pressure. This condition, which can cause symptoms like dizziness, nausea, and even fainting, poses a direct threat to the lives of both the mother and her unborn child.
Spinal anesthesia is the most common anesthetic used in Somalia. Its widespread use is due to its low cost and general safety profile. However, the study’s data reveals that its application in the Somali context yields a complication rate far exceeding that of other low- and middle-income countries. This 79% rate is significantly higher than those reported in nations like Ethiopia, Pakistan, and Colombia, suggesting that more than just the type of anesthesia is at play.
Beyond Medical Technique: A System Under Pressure
The high rate of complications points to a fundamental issue within Somalia’s healthcare infrastructure. While the spinal anesthesia itself can cause blood pressure drops, the study suggests that systemic weaknesses are a major contributing factor. According to Dr. Abdullahi Said Xashi of the hospital, complications are not just related to the procedure but also to the mother’s physiological state. His recommendations for prevention highlight potential gaps in standard care: he mentions that simply turning the mother to her left side and providing ample fluids before the operation can help prevent complications. The fact that these simple preventative measures need to be specifically recommended suggests that they may not be standard practice.
This situation reveals a healthcare system struggling to meet the demands of its population. The lack of proper pre-screening, consistent protocols, and a sufficient number of specialized medical professionals may all be contributing to the elevated risk. The study, therefore, serves as a powerful call to action.
The findings underscore the urgent need for a renewed focus on maternal health in Somalia. Experts who reviewed the study stress that investment is needed not just in medicines, but in the entire system. This includes enhancing pre-natal care to ensure mothers are properly screened for health risks before childbirth, as well as providing more robust training for medical staff.
The presence of a specialist during surgery to monitor and manage blood pressure is also highlighted as a critical need.
While the World Health Organization notes that the number of global cesarean sections is on the rise—with 88% of these procedures occurring in low- and middle-income countries—the unique challenges facing Somali mothers cannot be overlooked. The high rate of low blood pressure during C-sections is not merely a medical anomaly; it is a clear indicator that the health system requires a targeted and comprehensive intervention to better protect mothers and babies.
Health
Reviving Ancient Wisdom: Bacteria as Cancer-Fighting Tools Gain Ground

Harnessing bacteria to battle cancer: A fresh perspective on ancient methods promises a new era in oncology.
The concept of using bacteria to fight cancer, a method pioneered in the 19th century by William B. Coley, is undergoing a revolutionary resurgence. With advancements in genetic engineering and synthetic biology, scientists are transforming ordinary bacteria into targeted cancer-fighting agents, offering new hope in the battle against some of the most challenging malignancies.
Historically viewed with skepticism due to safety concerns and the dominance of traditional therapies like chemotherapy, bacteria-based cancer treatments are now recognized for their unique ability to thrive within the hostile tumor microenvironment. This niche, characterized by low oxygen levels, acidity, and dead tissue, provides an ideal breeding ground for certain bacteria, turning them into potent anti-cancer agents.
The resurgence of this approach is driven by the ability to genetically modify bacteria to safely target and kill tumor cells without harming healthy tissue. Modern techniques allow for precise control over bacterial behavior within tumors, enhancing their ability to stimulate the immune system against cancer cells effectively.
Despite the challenges of integrating live bacteria into therapeutic protocols—such as ensuring safety and controlling bacterial spread—the potential benefits are compelling. The engineered bacteria can produce and deliver anti-cancer compounds directly within the tumor, overcoming some of the limitations faced by conventional treatments, such as non-specific toxicity and difficulty reaching deep-seated tumor cells.
Promising research suggests that these microbial therapies could be particularly effective against solid tumors that are poorly served by existing options, such as ovarian, colon, and metastatic breast cancers. By combining these “bug drugs” with standard treatments, such as immunotherapy, there is potential to enhance efficacy and reduce side effects.
The ongoing development of bacterial cancer therapies is supported by recent successful preclinical trials, which show bacteria not only selectively colonizing tumors but also shrinking or even eliminating them in some cases. These results point to a future where bacteria-based therapies could play an integral role in a multi-modal cancer treatment strategy, providing a complementary approach to traditional therapies.
As the field advances, the focus on human trials will be crucial to determine the effectiveness of these therapies in controlling or eradicating cancer and understanding their potential side effects. The road ahead is paved with both promise and challenges, but the integration of historical insights with modern biotechnology may soon lead to breakthroughs in cancer treatment, offering hope to those battling this relentless disease.
-

 Minnesota2 months ago
Minnesota2 months agoFraud Allegations Close In on Somalia’s Top Diplomats
-

 Middle East2 months ago
Middle East2 months agoTurkey’s Syria Radar Plan Triggers Israeli Red Lines
-

 Editor's Pick2 months ago
Editor's Pick2 months agoWhy India Is Poised to Become the Next Major Power to Recognize Somaliland
-

 ASSESSMENTS2 months ago
ASSESSMENTS2 months agoSomalia’s Risky Pact with Pakistan Sparks Regional Alarm
-

 Analysis2 months ago
Analysis2 months agoTurkey’s Expanding Footprint in Somalia Draws Parliamentary Scrutiny
-

 Analysis2 months ago
Analysis2 months agoRED SEA SHOCKER: TURKEY’S PROXY STATE RISES—AND ISRAEL IS WATCHING
-

 Somaliland1 month ago
Somaliland1 month agoF-35s Over Hargeisa: The Night Somaliland’s Sovereignty Went Supersonic
-

 Somalia2 months ago
Somalia2 months agoIs Somalia’s Oil the Price of Loyalty to Turkey? MP Blows Whistle on Explosive Oil Deal